| 病例1 | |
|---|---|
 | 品种:短毛猫 |
| 年龄:8岁 | |
| 性别:雄 | |
| 是否绝育:是 | |
| 诊断:梗阻性输尿管结石 | |
01 主诉及病史
排尿困难、血尿、腹腔积液和皮下肿胀。
6周前曾因梗阻性输尿管结石而接受输尿管切开术和单侧经皮输尿管分流术(SUB)。
02 检查
腹腔积液检测后是一种伴有低度炎症和积液的渗出液,尿培养呈阴性。美洛昔康(0.05 mg/kg 口服q24h)和丁丙诺啡(0.01 mg/kg皮下注射q12h)未能缓解排尿困难。血清肌酐为131 µmol/l(71-212)。
SUB系统位置适当,无阻塞或渗漏。右侧输尿管近端扩张至先前输尿管切开的水平。通过 SUB端口注入稀释的碘海醇进行肾盂造影,结果显示右侧输尿管在该水平存在梗阻。
03 手术
输尿管切开术显示有纤维组织,管腔内无阻塞物。进行了输尿管支架植入术(如下所述),并移除了整个SUB系统。移除肾造瘘管后,用可吸收缝合线缝合肾造瘘管边缘。
04 预后
术后立即解决了排尿问题。
术后5周,腹腔积液和皮下肿胀经超声检查证实已经消退。
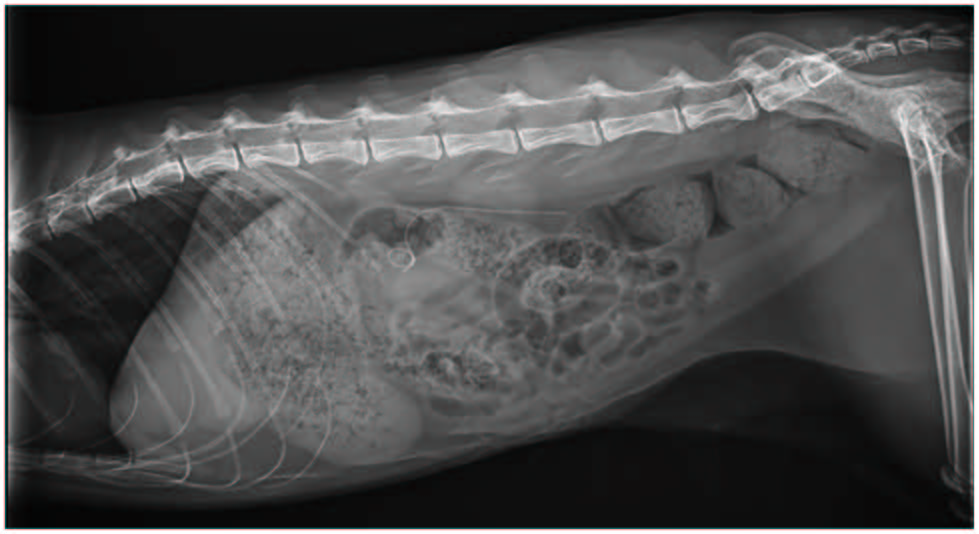
术后8个月,下尿路体征没有复发。腹部X光片显示支架位置没有变化。支架末端的超声检查未发现异常。血清肌酐为109 µmol/l。
| 病例2 | |
|---|---|
 | 品种:短毛猫 |
| 年龄:5岁 | |
| 性别:雌 | |
| 是否绝育:是 | |
| 诊断:梗阻性输尿管结石 | |
05 检查
氮质血症,腹部超声符合右侧梗阻性输尿管结石,包括肾盂和输尿管近端扩张以及高回声输尿管结石。血清肌酐为757 µmol/l(69-160)。
06 手术
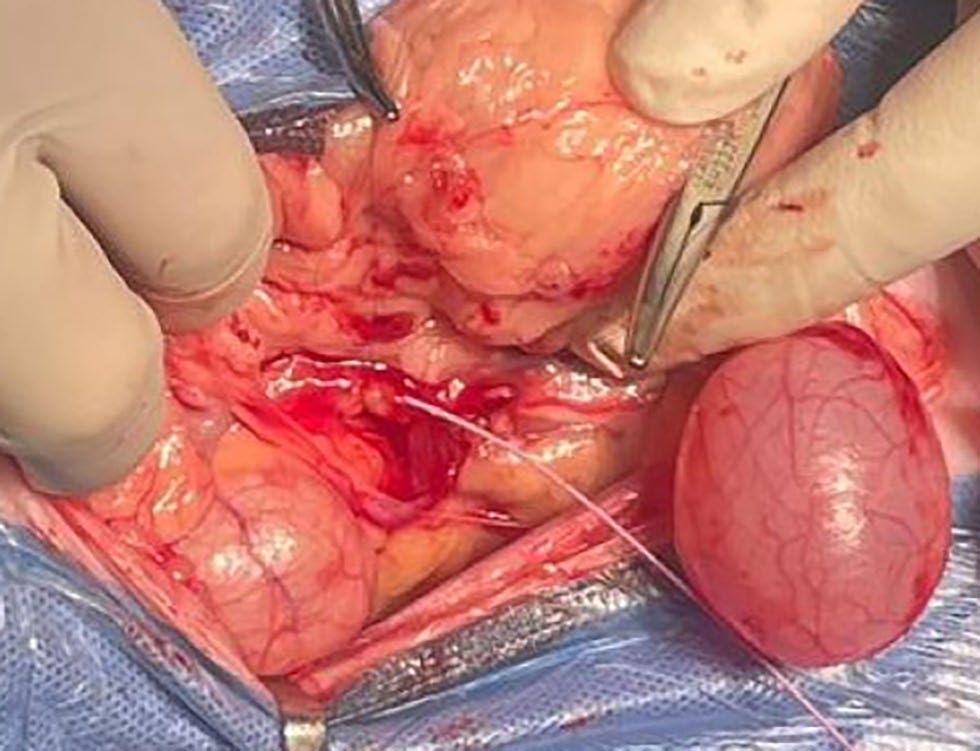
术中在右侧输尿管内触及输尿管结石,距离肾脏三分之一的位置,输尿管近端扩张。进行了输尿管切开术,取出了输尿管结石。进行了输尿管支架置入手术,如下所述。
在透视引导下,通过输尿管切口将0.018英寸亲水导丝逆行导入肾盂(下图)。在导丝上方将2+F支架导入肾盂。取出导线后,切割支架远端,长度足以桥接输尿管切开部位。将支架末端导入输尿管远端,并推进到输尿管切口外约1厘米处。使用USP 6-0缝线以简单间断方式完成输尿管切口闭合。在病例1中,通过SUB端口进行了术中肾盂造影,以确认支架置入后输尿管是否通畅。


07 预后
术后6周氮质血症有所改善,血清肌酐降至186 mmol/l(69-160),血清尿素降至 24.0 mmol/l(5.8-11.5)。术后7复查临床症状正常。腹部X光片显示支架位置无变化(下图)。支架末端的超声检查未发现异常。血清肌酐为139 µmol/l。

08 讨论
腔内输尿管支架和肾静脉旁路导管已成为治疗猫梗阻性输尿管结石的标准方法[1-9]。这两种方法都能减少过去使用的技术(包括输尿管切开术、新输尿管囊肿切除术、输尿管部分切除术和输尿管肾切除术)所带来的并发症[3,10,11]。然而,仍有报道称这些新方法的并发症发生率很高。
一项比较研究报告称,双鱼尾支架并发症的发生率较高,包括下尿路体征、支架梗阻和尿崩症[12]。下尿路体征(包括排尿困难和尿频)的发生率在20%-48%之间[1,2,12-14]。其他并发症包括支架移位、输尿管炎、肾盂肾炎和需要更换支架,据报道多达27%的猫需要更换支架[1,2,12-14]。
与经皮输尿管分流术(SUB)相关的并发症也很常见,包括SUB闭塞、扭结、渗漏、感染和矿化[4,5,8,12],据一项研究报告称主要并发症发生率为48%[5],因此一些学者开始探索输尿管膀胱造口术,以限制异物植入和传统技术的并发症发生率[15]。
腔内支架可以逆行放置,通过膀胱切开术(开放手术或内镜手术),也可以顺行放置,通过肾脏,还可以双向放置,通过输尿管切开术切口[1-3,10,12-14]。猫输尿管直径较小,尤其是在膀胱输尿管交界处,这使得置管复杂化,而管腔阻塞或狭窄又会增加置管难度[10,13]。因此,腔内输尿管支架置入术可能导致手术时间延长、额外的手术创伤和无法成功置入的情况[3,13]。
下尿路体征和侧腹疼痛是腔内支架置入术后常见的并发症[1],限制了其广泛应用[3,14]。猫的尿道近端位置导致尿道和三叉神经粘膜受到膀胱内支架的刺激[13]。人类输尿管支架患者中约80%-90%的患者会出现排尿困难、尿急和侧腹疼痛等症状[16]。
在人体中,下尿路体征与支架直径[17]和长度[18,19]有关,尤其是支架终端穿过膀胱中线[19,20]或在输尿管内终止[21-23]的位置。疼痛与膀胱输尿管反流和肾盂内压升高有关,尤其是在排尿时[18,21,24],因为支架绕过输尿管肾盂交界处并阻碍输尿管蠕动。
最近有报道称,在人类体内短期放置腔内输尿管支架时,输尿管远端留在输尿管内可显著减轻下尿路症状并改善生活质量[21-23]。本报告描述了在两只猫身上进行的改良腔内输尿管支架植入术。
除了输尿管支架植入术或旁路术外,输尿管切开术对猫输尿管结石症的价值尚未得到充分证实。输尿管切开术可解除管腔内梗阻,并获得结石和微生物分析标本,但存在并发症风险,包括漏尿、输尿管梗阻、狭窄和粘连[26]。
在最近一份关于SUB的报告中,输尿管切开术被认为会延长麻醉和手术时间,但不会影响存活率[27]。输尿管切口支架植入术可避免管壁软组织炎症造成的管腔阻塞、输尿管切口闭合造成的输尿管解剖结构改变或狭窄[26]。这些优点都与输尿管切开部位有关。
除固定外,支架是否需要沿输尿管长度进一步延伸尚未确定。事实上,横跨整个输尿管的支架会造成膀胱内支架肿块,使输尿管与膀胱交界处失去功能,并影响输尿管蠕动。在猪模型中研究了腔内输尿管支架对生理和尿动力学的影响,结果显示存在明显的膀胱肾压力传导和反流,输尿管普遍扩张,这被认为是对低效蠕动的反应性扩张[28]。对未患病猪输尿管进行的其他尿动力学研究表明,腔内支架导致输尿管阻塞的方式与支架的直径和长度有关[16,29]。
市售腔内支架的设计支持膀胱镜置入和取出,尽管有报道称猫科动物不太容易做到这一点[13]。卷曲的末端限制了向任一方向移位的可能性[16]。据报道,少数猫的输尿管支架发生过逆行和顺行移位,而人类很少发生逆行移位[1,13,30,31]。人类文献中没有输尿管腔内支架逆行移位的报道[22,23]。在本病例中,为防止远端移位,保留了支架的卷曲端。虽然支架在腔内终止对术后移位的影响尚不清楚,但在本病例中,术后7个月和8个月未观察到移位。
腔内支架植入术的技术难度是限制其广泛应用的一个因素,并可能导致输尿管创伤[3,10,13,32]。支架可经膀胱逆行插入或经肾脏顺行插入,但也有报道称,经输尿管切开术置入支架的同时进行膀胱切开术,将支架推进膀胱并逆行进入肾脏[1,10,13]。
在本病例中,支架通过输尿管切开术直接推进到肾盂。通过在梗阻部位近端进行输尿管扩张、输尿管切口靠近肾盂、避免支架穿过输尿管与肾小管交界处和输尿管梗阻部位等方法简化了支架的放置。避免了支架直径与未扩张的远端输尿管之间的不匹配。
在两个病例中,输尿管近端都出现了明显的扩张。病例1之前放置的SUB允许进行前行肾盂造影,以确定腔内支架放置和输尿管切开关闭后的输尿管通畅情况。在病例2中,支架末端以外的输尿管通畅性尚未确定,而是根据其术中正常外观推测的。在未来的病例中,可能需要通过输尿管切开术进行术中输尿管造影,以排除更广泛的输尿管支架置入或输尿管分流的需要。
虽然在这两个病例的超声随访中均未发现明显的输尿管病变,但支架末端留在输尿管内对输尿管的物理影响尚不清楚。支架末端留在输尿管内也无法在膀胱镜或透视引导下进行微创移除,如果需要移除,只能采用输尿管切开术或经肾方法。
输尿管切开术伴随着尿液渗漏[1,12]、进一步梗阻和狭窄的风险;不过,由于移除支架所需的输尿管切开术规模较小,而且腔内支架植入术会导致输尿管扩张,因此有望将这些风险降至最低。有报道称,在人体中使用带回收绳的支架可提供一种创伤较小的移除方法[21-23,33]。类似的方法可能适用于未来猫科动物输尿管腔内支架的设计。
参考文献
1. Kulendra NJ, Syme H, Benigni L, et al. Feline double pigtail ureteric stents for management of ureteric obstruction: short- and long-term follow-up of 26 cats. J Feline Med Surg 2014; 16: 985–991.
2. Manassero M, Decambron A, Viateau V, et al. Indwelling double pigtail ureteral stent combined or not with surgery for feline ureterolithiasis: complications and outcome in 15 cases. J Feline Med Surg 2014; 16: 623–630.
3. Schwartz P. Current concepts in urinary surgery. Vet Clin North Am Small Anim Pract 2022; 52: 387–417.
4. Berent AC, Weisse CW, Bagley DH, et al. Use of a subcutaneous ureteral bypass device for treatment of benign ureteral obstruction in cats: 174 ureters in 134 cats (2009–2015). J Am Vet Med Assoc 2018; 253: 1309–1327.
5. Kulendra NJ, Borgeat K, Syme H, et al. Survival and complications in cats treated with subcutaneous ureteral bypass. J Small Anim Pract 2021; 62: 4–11.
6. Palm CA, Culp WT. Nephroureteral obstructions: the use of stents and ureteral bypass systems for renal decompression. Vet Clin North Am Small Anim Pract 2016; 46: 1183–1192.
7. Vrijsen E, Devriendt N, Mortier F, et al. Complications and survival after subcutaneous ureteral bypass device placement in 24 cats: a retrospective study (2016–2019). J Feline Med Surg 2021; 23: 759–769.
8. Wuillemin F, Vachon C, Beauchamp G, et al. Subcutaneous ureteral bypass device placement in 81 cats with benign ureteral obstruction (2013–2018). J Vet Intern Med 2021; 35: 2778–2786.
9. Lulich JP, Berent AC, Adams LG, et al. ACVIM small animal consensus recommendations on the treatment and prevention of uroliths in dogs and cats. J Vet Intern Med 2016; 30: 1564–1574.
10. Culp WT, Palm CA, Hsueh C, et al. Outcome in cats with benign ureteral obstructions treated by means of ureteral stenting versus ureterotomy. J Am Vet Med Assoc 2016; 249: 1292–1300.
11. Berent AC, Weisse CW, Todd KL, et al. Use of locking-loop pigtail nephrostomy catheters in dogs and cats: 20 cases (2004–2009). J Am Vet Med Assoc 2012; 241: 348–357.
12. Deroy C, Rossetti D, Ragetly G, et al. Comparison between double-pigtail ureteral stents and ureteral bypass devices for treatment of ureterolithiasis in cats. J Am Vet Med Assoc 2017; 251: 429–437.
13. Berent AC, Weisse CW, Todd K, et al. Technical and clinical outcomes of ureteral stenting in cats with benign ureteral obstruction: 69 cases (2006–2010). J Am Vet Med Assoc 2014; 244: 559–576.
14. Wormser C, Clarke DL, Aronson LR. Outcomes of ureteral surgery and ureteral stenting in cats: 117 cases (2006–2014). J Am Vet Med Assoc 2016; 248: 518–525.
15. Lorange M, Monnet E. Postoperative outcomes of 12 cats with ureteral obstruction treated with ureteroneocystostomy. Vet Surg 2020; 49: 1418–1427.
16. Tolley D. Ureteric stents, far from ideal. Lancet 2000; 356: 872–873.
17. Nestler S, Witte B, Schilchegger L, et al. Size does matter: ureteral stents with a smaller diameter show advantages regarding urinary symptoms, pain levels and general health. World J Urol 2020; 38: 1059–1063.
18. Al-Kandari AM, Al-Shaiji TF, Shaaban H, et al. Effects of proximal and distal ends of double-J ureteral stent position on postprocedural symptoms and quality of life: a randomized clinical trial. J Endourol 2007; 21: 698–702.
19. Bao X, Sun F, Yao H, et al. Distal end of double-J ureteral stent position on ureteral stent-related symptoms: a systematic review and meta-analysis. Front Surg 2022; 9.
20. Inn FX, Ahmed N, Hou LG, et al. Intravesical stent position as a predictor of quality of life in patients with indwelling ureteral stent. Int Urol Nephrol 2019; 51: 1949–1953.
21. Ho CH, Liu SP, Wang CW, et al. Complete intraureteral stent placement reduces stent-related symptoms: systemic review and meta-analysis. J Formos Med Assoc 2022; 121: 2308–2316.
22. Tzou KY, Chen KC, Wu CC, et al. The intraureteral placement of the stent’s distal end decreases stent-related urinary symptoms: a prospective randomized clinical trial. World J Urol 2022; 40: 2129–2134.
23. Yoshida T, Inoue T, Taguchi M, et al. Efficacy and safety of complete intraureteral stent placement versus conventional stent placement in relieving ureteral stent related symptoms: a randomized, prospective, single blind, multicenter clinical trial. J Urol 2019; 202: 164–170.
24. Duvdevani M, Chew BH, Denstedt JD. Minimizing symptoms in patients with ureteric stents. Curr Opin Urol 2006; 16: 77–82.
25. Nicoli S, Morello E, Martano M, et al. Double-J ureteral stenting in nine cats with ureteral obstruction. Vet J 2012; 194: 60–65.
26. Kyles AE, Hardie EM, Wooden BG, et al. Management and outcome of cats with ureteral calculi: 153 cases (1984–2002). J Am Vet Med Assoc 2005; 226: 937–944.
27. Butty EM, Labato MA. Subcutaneous ureteral bypass device placement with intraoperative ultrasound guidance, with or without microsurgical ureterotomy, in 24 cats. J Feline Med Surg 2021; 23: 1183–1191.
28. Ramsay JW, Payne SR, Gosling PT, et al. The effects of double J stenting on unobstructed ureters. An experimental and clinical study. Br J Urol 1985; 57: 630–634.
29. Payne SR, Ramsay JW. The effects of double J stents on renal pelvic dynamics in the pig. J Urol 1988; 140: 637–641.
30. Al-Hajjaj M. Upward migration of a double J ureteral stent in a boy: a rare case report. Ann Med Surg (Lond) 2022; 82.
31. Ahmed F, Alyhari Q, Ghabisha S, et al. Jejunal perforation and upward migration of double J stents during the cystoscopic procedure: a case report and review of literature. Pan Afr Med J 2022; 42.
32. Milligan M, Berent AC. Medical and interventional management of upper urinary tract uroliths. Vet Clin North Am Small Anim Pract 2019; 49: 157–174.
33. Lim KS, Law ZW, Chow MWL, etal. Peak stent discomfort occurs early and ureteral stent with distal loop design has less pain – a pilot prospective randomised single-blinded trial over 2 weeks. Asian J Urol 2020; 7: 357–362.