| 一般情况 | |
|---|---|
 | 品种:混种犬 |
| 年龄:16岁 | |
| 性别:雄 | |
| 是否绝育:否 | |
| 诊断:高致病性禽流感病毒感染 | |
01 主诉及病史
2023年6月因持续干咳、伴有轻度浆液性鼻涕就诊,无其他症状。
就诊前1周被从农村地区领养,既往健康状况不明。被领养后生活在小镇上,镇上大约有16000名居民。领养后的1周内吃干粮,没有食用新鲜或冷冻肉类。
在该犬居住地区没有关于野生或家养鸟类感染禽流感的报告。最近的野生鸟类A/H5N1确诊病例发生在该犬症状出现前不到1个月,地点分别距离该犬居住地约200公里和270公里。
02 检查
查体发现严重干咳,主人报告一天中多次咳嗽。颌下淋巴结肿大。体温37.7°C,心跳130次/分,呼吸24次/分,黏膜湿润呈粉红色,毛细血管再充盈时间<2秒,听诊时发现左心尖杂音,II/VI级,但未发现病理性肺音。
口服10 mg/kg阿莫西林和2.5 mg/kg克拉维酸治疗,同时皮下注射地塞米松0.05 mL/kg。治疗2天后症状没有改善。
进一步检查显示,血碱性磷酸酶活性为382 U/L(0-160),总蛋白7.99 g/dL(5.4-7.5),球蛋白49.3 g/L(25-45)。尿素和肌酐正常。除了血细胞比容36.6%(37-55)和红细胞5.16 M/µL(5.5-8.5)外,血细胞计数无异常。
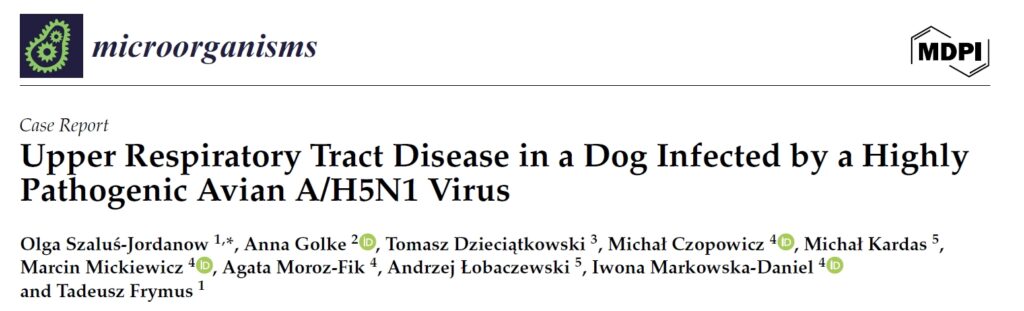
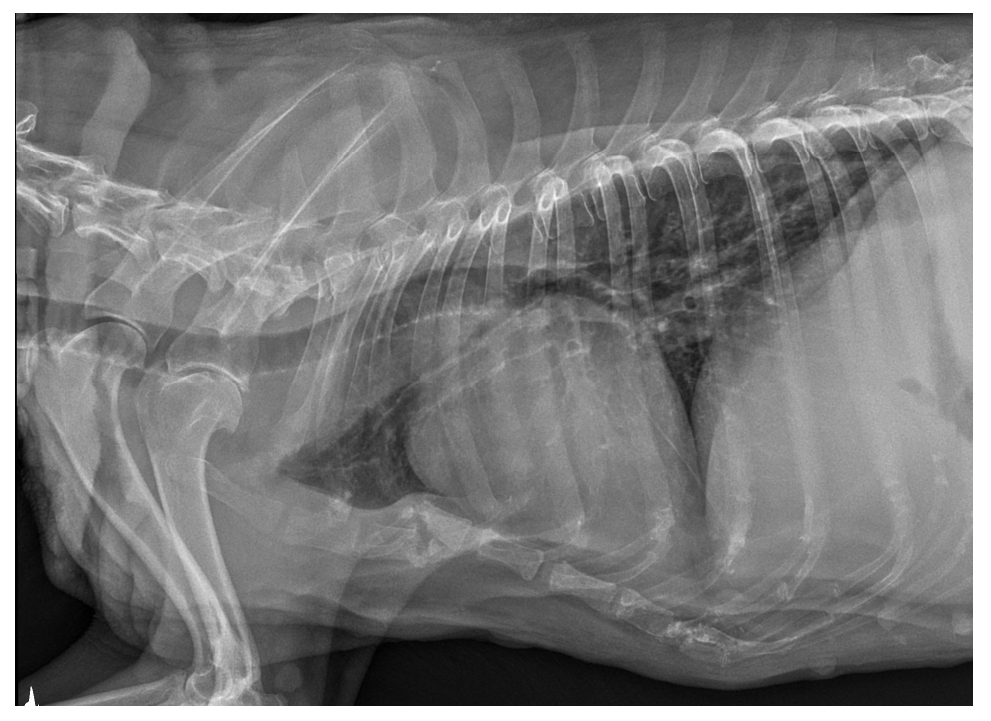
X光片上的肺实质图像未发现病理变化(下图)。
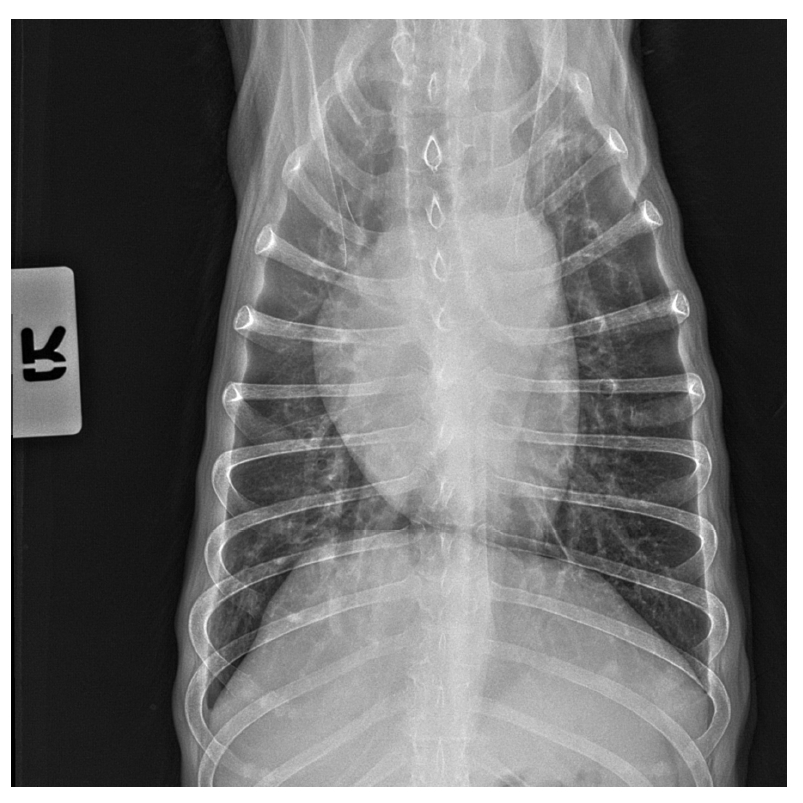
超声显示所有切面的肺部形态正常。胸膜线完整,存在A线伪影(下图)。还观察到滑动征。
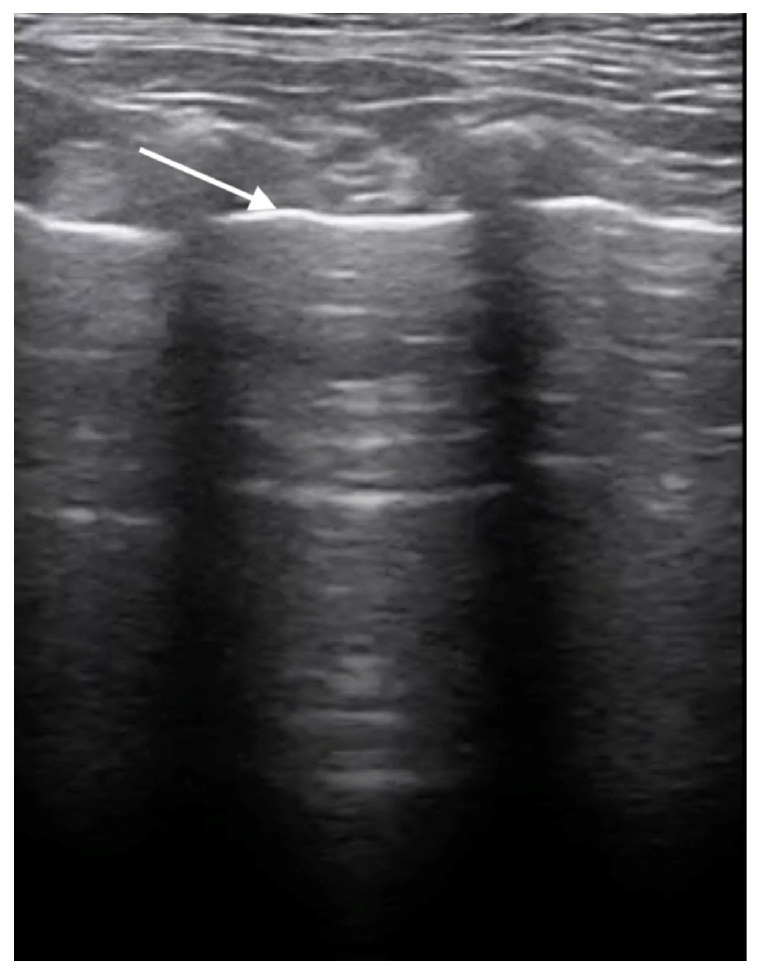
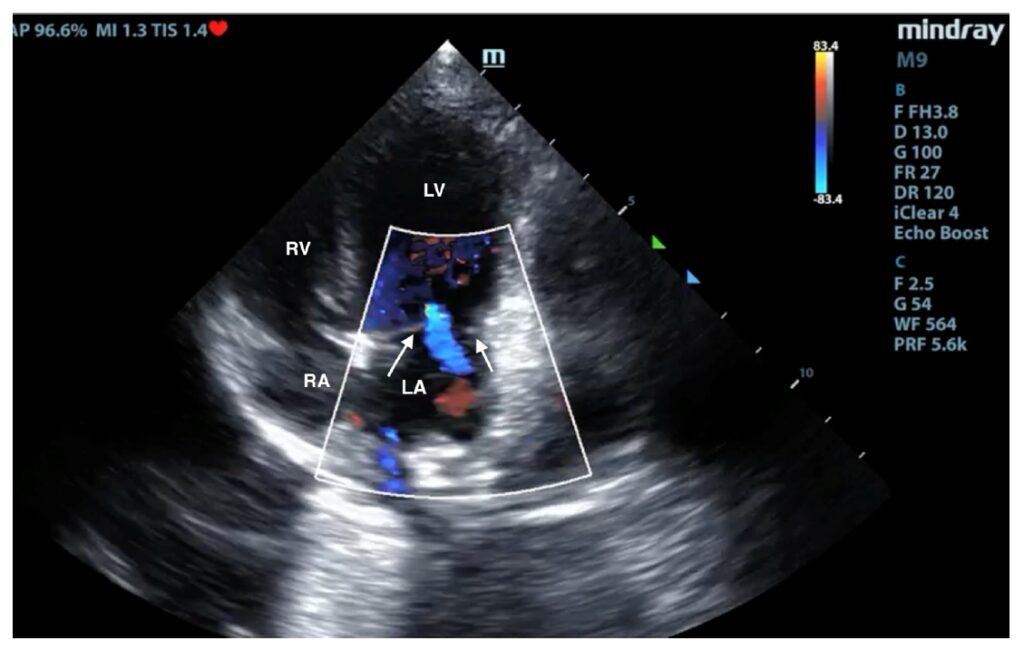
超声心动图显示二尖瓣瓣叶轻度增厚,瓣膜轻微反流(下图)。心腔大小在正常范围内,心肌收缩力正常。
用于病毒学检测的咽拭子是在临床检查时采集的。对甲型流感病毒亚型H1N1、H3N2、H5N1、乙型流感病毒和SARS-CoV-2进行了分子诊断。结果显示流感病毒甲型H5N1(A/H5N1)PCR结果阳性。
03 治疗
在治疗4天无效后,根据流感PCR检测结果,将阿莫西林加克拉维酸改为马勃沙星2 mg/kg每天一次加头孢韦辛8 mg/kg皮下注射。作为止咳药,丁吗啡诺的剂量为0.2 mg/kg每天三次。
04 预后
用药后咳嗽减轻,但鼻腔内的浆液性分泌物变成了脓性。整个疗程持续了18天,咳嗽最终缓解。该犬感染A/H5N1病毒后完全恢复了健康。
05 讨论
流感是一种由正粘病毒引起的传染性极强的上呼吸道感染,已成为犬的健康问题。在犬科动物中发现了几种甲型流感病毒亚型,这些病毒株最初与不同的宿主物种相关。其中包括主要影响人类和猪的A/H1N1病毒,最初与鸟类相关的 A/H3N2、A/H3N6、A/H5N2、A/H9N2和A/H10N8,以及源自马流感病毒的A/H3N8[1-7]。
只有A/H3N8和A/H3N2两种亚型在犬身上适应后成为犬流感病毒。在美国,第一种由马传播给犬的病毒自2000年代初开始在佛罗里达州的赛灰狗中流行,随后传播到美国的其他犬种和地区[2,8],可能在2016年左右绝迹[9]。
2007年澳大利亚发生马流感疫情时,这种马病毒也曾传播给犬[10]。到2006年,A/H3N2病毒(很可能源于禽类)在中国或韩国[11]在犬身上发现,并在那里诱发了数次犬地方性疫情,后来又被传播到美国[12]。
A/H3N8和A/H3N2犬流感病毒均可引起急性上呼吸道感染,表现为发烧、咳嗽和流鼻涕,但只有少数犬病情严重。虽然继发细菌感染可能导致肺炎或其他并发症,但大多数患者在1-3周后即可康复,死亡率通常低于1%[13]。因此,这些病原体与人类和其他多种哺乳动物和鸟类的“季节性”甲流病毒一起被归类为“低致病性”病毒。
“高致病性”甲流病毒几乎只出现在鸟类中,可诱发严重的全身感染,不仅影响肺部,还影响许多其他器官,导致家禽和野生鸟类大量死亡。最重要的高致病性亚型是1996年在东南亚和21世纪初出现的A/H5N1病毒,它在该地区引发了大规模、长时间的流行[14]。
随后,这一流行病扩展到非洲、欧洲和最近的美洲[15]。在极少数情况下,哺乳动物也受到影响,其中包括870多人,死亡率超过50%[16]。饲喂新鲜或冷冻的受污染鸟类尸体、狩猎或与鸟类的其他接触导致伴侣动物[2,17-21]和野猫[19]出现零星但通常非常严重的病例。
尽管20多年来A/H5N1病毒一直在亚洲、欧洲和非洲的鸟类中流行,但迄今为止猫感染高致病性禽流感的病例非常罕见,而且通常是孤立的。2023年,韩国仅有两家猫收容所爆发大规模疫情,最有可能的原因是猫粮中的鸭肉受到污染[22]。在波兰的几个地区,2023年夏季发生了多起饲养的家猫感染高致病性禽流感的病例,其中既有室外动物,也有室内动物[23,24]。同样不能排除禽肉受污染的可能性[23,25]。
至少有34例猫病例得到确诊,其中包括一只人工饲养的狞猫。然而,受感染猫的真实数量更高,至少在作者的实验室中,确诊过几例猫感染病例,还有4例雪貂感染病例和一例犬感染病例[26]。
有证据表明,犬也可能无症状地携带A/H5N1病毒[2,27]。然而,与猫相比,迄今为止几乎没有关于犬感染A/H5N1病毒后自发发病的描述。因此,本病例报告介绍了2023年夏季波兰首例感染A/H5N1病毒的犬的临床病程、肺部超声检查及其他发现。
本病例证实,在极少数情况下,A/H5N1病毒也会诱发犬的严重呼吸道疾病。有些犬感染后无症状[35],有些则表现出轻微症状,如短暂发烧[34],甚至出现致命疾病[20]。
最近,在家禽爆发2.3.4.4b支系高致病性禽流感A/H5N1疫情期间,意大利一家农场发现了5只血清反应呈阳性的健康狗。从禽类中分离出的病毒在PB2基因中有T271A突变,这是病毒适应哺乳动物的标志[38]。
Maas等人[35]使用标记的A/H5N1病毒进行的研究表明,病原体能够附着在犬的上呼吸道和下呼吸道组织上。这表明,正如Chen等人[37]报道的那样,犬在将高致病性禽流感从禽类传播给人类的过程中可能扮演中间宿主的角色。
波兰和大多数欧洲国家一样,对出现呼吸道症状的犬不进行常规流感检测。本病例证实,在欧洲,由于过去几年高致病性禽流感疫情在欧洲很常见,犬可能患上由A/H5N1病毒诱发的疾病。因此,在禽类高致病性禽流感流行的地区,不仅要对猫进行鉴别诊断,也要对犬进行鉴别诊断,尤其是呼吸道疾病患者。
文献来源:Szaluś-Jordanow O, Golke A, Dzieciątkowski T, Czopowicz M, Kardas M, Mickiewicz M, Moroz-Fik A, Łobaczewski A, Markowska-Daniel I, Frymus T. Upper Respiratory Tract Disease in a Dog Infected by a Highly Pathogenic Avian A/H5N1 Virus. Microorganisms. 2024 Mar 29;12(4):689.
参考文献
1. Crawford P.C., Dubovi E.J., Castleman W.L., Stephenson I., Gibbs E.P.J., Chen L., Smith C., Hill R.C., Ferro P., Pompey J., et al. Transmission of equine influenza virus to dogs. Science. 2005;21:482–485.
2. Rivailler P., Ijeoma Perry I.P., Jang Y., Davis C.T., Chen L., Dubovi E.J., Donis R.O. Evolution of canine and equine influenza (H3N8) viruses co-circulating between 2005 and 2008. Virology. 2010;5:71–79.
3. Songserm T., Amonsin A., Jam-on R., Sae-Heng N., Meemak N., Pariyothorn N., Payungporn S., Theamboonlers A., Poovorawan Y. Avian Influenza H5N1 in Naturally Infected Domestic Cat. Emerg. Infect. Dis. 2006;12:681–683.
4. Zhu M., Zeng H., He J., Zhu Y., Wang P., Guo J., Guo J., Zhou H., Qin Y., Ouyang K., et al. Reassortant H9N2 canine influenza viruses containing the pandemic H1N1/2009 ribonucleoprotein complex circulating in pigs acquired enhanced virulence in mice. Virology. 2024;589:109927.
5. Meng B., Li H., Feng C., Guo W., Feng Y., Zhu D., Chen H., Zhang Y. Emergence of a novel reassortant H3N6 canine influenza virus. Front. Microbiol. 2023;11:1186869.
6. Zhan G.J., Ling Z.S., Zhu Y.L., Jiang S.J., Xie Z.J. Genetic characterization of a novel influenza A virus H5N2 isolated from a dog in China. Vet. Microbiol. 2012;23:409–416.
7. Su S., Qi W., Zhou P., Xiao C., Yan Z., Cui J., Jia K., Zhang G., Gray G.C., Liao M., et al. First evidence of H10N8 Avian influenza virus infections among feral dogs in live poultry markets in Guangdong province, China. Clin. Infect. Dis. 2014;1:748–750.
8. Anderson T.C., Bromfield C.R., Crawford P.C., Dodds W.J., Gibbs E.P., Hernandez J.A. Serological evidence of H3N8 canine influenza-like virus circulation in USA dogs prior to 2004. Vet. J. 2012;191:312–316.
9. Wasik B.R., Rothschild E., Voorhees I.E.H., Reedy S.E., Murcia P.R., Pusterla N., Chambers T.M., Goodman L.B., Holmes E.C., Kile J.C., et al. Understanding the divergent evolution and epidemiology of H3N8 influenza viruses in dogs and horses. Virus Evol. 2023;18:vead052.
10. Crispe E., Finlaison D.S., Hurt A.C., Kirkland P.D. Infection of dogs with equine influenza virus: Evidence for transmission from horses during the Australian outbreak. Aust. Vet. J. 2011;89:27–28.
11. Zhu H., Hughes J., Murcia P.R. Origins and evolutionary dynamics of H3N2 canine influenza virus. J. Virol. 2015;89:5406–5418.
12. Voorhees I.E.H., Glaser A.L., Toohey-Kurth K., Newbury S., Dalziel B.D., Dubovi E.J., Poulsen K., Leutenegger C., Willgert K.J.E., Brisbane-Cohen L., et al. Spread of canine influenza A(H3N2) virus, United States. Emerg. Infect. Dis. 2017;23:1950–1957.
13. Wasik B.R., Voorhees I.E.H., Parrish C.R. Canine and Feline Influenza. Cold Spring Harb. Perspect. Med. 2021;11:a038562.
14. Webster R.G., Guan Y., Poon L., Krauss S., Webby R., Govorkovai E., Peiris M. The spread of the H5N1 bird flu epidemic in Asia in 2004. Arch. Virol. Suppl. 2005;19:17–29.
15. Adlhoch C., Fusaro A., Gonzales J.L., Kuiken T., Mirinavičiūtė G., Niqueux É., Ståhl K., Staubach C., Terregino C., Willgert K., et al. European Food Safety Authority; European Centre for Disease Prevention and Control; European Union Reference Laboratory for Avian Influenza; Avian influenza overview September-December 2023. EFSA J. 2023;21:e8539.
16. WHO Cumulative Number of Confirmed Human Cases for Avian Influenza A(H5N1) [(accessed on 11 January 2024)].
17. Kuiken T., Rimmelzwaan G., van Riel D., van Amerongen G., Baars M., Fouchier R., Osterhaus A. Avian H5N1 Influenza in Cats. Science. 2004;306:241.
18. Thiry E., Zicola A., Addie D., Egberink H., Hartmann K., Lutz H., Poulet H., Horzinek M. Highly pathogenic avian influenza H5N1 virus in cats and other carnivores. Vet. Microbiol. 2007;122:25–31.
19. Keawcharoen J., Oraveerakul K., Kuiken T., Fouchier R.A.M., Amonsin A., Payungporn S., Noppornpanth S., Wattanodorn S., Theambooniers A., Tantilertcharoen R., et al. Avian Influenza H5N1 in Tigers and Leopards. Emerg. Infect. Dis. 2004;10:2189–2191.
20. Songserm T., Amonsin A., Jam-on R., Sae-Heng N., Pariyothorn N., Payungporn S., Theamboonlers A., Chutinimitkul S., Thanawongnuwech R., Poovorawan Y. Fatal avian influenza A H5N1 in a dog. Emerg. Infect. Dis. 2006;12:1744–1747.
21. Hiono T., Kobayashi D., Kobayashi A., Suzuki T., Satake Y., Harada R., Matsuno K., Sashika M., Ban H., Kobayashi M., et al. Virological, pathological, and glycovirological investigations of an Ezo red fox and a tanuki naturally infected with H5N1 high pathogenicity avian influenza viruses in Hokkaido, Japan. Virology. 2023;578:35–44.
22. Kim Y., Fournié G., Métras R., Song D., Donnelly C.A., Pfeiffer D.U., Nouvellet P. Lessons for cross-species viral transmission surveillance from highly pathogenic avian influenza Korean cat shelter outbreaks. Nat. Commun. 2023;31:6958.
23. Szaluś-Jordanow O., Golke A., Dzieciątkowski T., Chrobak-Chmiel D., Rzewuska M., Czopowicz M., Sapierzyński R., Kardas M., Biernacka K., Mickiewicz M., et al. A Fatal A/H5N1 Avian Influenza Virus Infection in a Cat in Poland. Microorganisms. 2023;9:2263.
24. Domańska-Blicharz K., Świętoń E., Świątalska A., Monne I., Fusaro A., Tarasiuk K., Wyrostek K., Styś-Fijoł N., Giza A., Pietruk M., et al. Outbreak of Highly Pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b Virus in Cats, Poland, June to July 2023. Euro Surveill. 2023;28:2300366.
25. Rabalski L., Milewska A., Pohlmann A., Gackowska K., Lepionka T., Szczepaniak K., Swiatalska A., Sieminska I., Arent Z., Beer M., et al. Emergence and Potential Transmission Route of Avian Influenza A (H5N1) Virus in Domestic Cats in Poland, June 2023. Euro Surveill. 2023;28:2300390.
26. Golke A., Dzieciątkowski T., Szaluś-Jordanow O., Jańczak D., Sapierzyński R., Moroz-Fik A., Frymus T. Highly pathogenic A/H5N1 influenza virus infections in cats, ferrets and dogs in Poland and other countries. Mag. Weter. 2023;4:1–5.
27. Amonsin A., Songserm T., Chutinimitkul S., Jam-On R., Sae-Heng N., Pariyothorn N., Payungporn S., Theamboonlers A., Poovorawan Y. Genetic analysis of influenza A virus (H5N1) derived from domestic cat and dog in Thailand. Arch. Virol. 2007;152:1925–1933.
28. Stefańska I., Dzieciatkowski T., Brydak L.B., Romanowska M. Application of three duplex real-time PCR assays for simultaneous detection of human seasonal and avian influenza viruses. Arch. Virol. 2013;158:1743–1753.
29. Briand F.X., Souchaud F., Pierre I., Beven V., Hirchaud E., Hérault F., Planel R., Rigaudeau A., Bernard-Stoecklin S., Van der Werf S., et al. Highly Pathogenic Avian Influenza A(H5N1) Clade 2.3.4.4b Virus in Domestic Cat, France, 2022. Emerg. Infect. Dis. 2023;29:1696.
30. Rijks J.M., Hesselink H., Lollinga P., Wesselman R., Prins P., Weesendorp E., Engelsma M., Heutink R., Harders F., Kik M., et al. Highly pathogenic avian influenza A(H5N1) virus in wild red foxes, The Netherlands, 2021. Emerg. Infect. Dis. 2021;27:2960.
31. Tammiranta N., Isomursu M., Fusaro A., Nylund M., Nokireki T., Giussani E., Zecchin B., Terregino C., Gadd T. Highly pathogenic avian influenza A (H5N1) virus infections in wild carnivores connected to mass mortalities of pheasants in Finland. Infect. Genet. Evol. 2023;111:105423.
32. Lindh E., Lounela H., Ikonen N., Kantala T., Savolainen-Kopra C., Kauppinen A., Osterlund P., Kareinen L., Katz A., Nokireki T., et al. Highly pathogenic avian influenza A(H5N1) virus infection on multiple fur farms in the South and Central Ostrobothnia regions of Finland, July 2023. Euro Surveill. 2023;28:2300400.
33. Agüero M., Monne I., Sánchez A., Zecchin B., Fusaro A., Ruano M.J., Del Valle Arrojo M., Fernández-Antonio R., Souto A.M., Tordable P., et al. Highly pathogenic avian influenza A(H5N1) virus infection in farmed minks, Spain, October 2022. Euro Surveill. 2023;28:2300001.
34. Giese M., Harder T.C., Teifke J.P., Klopfleisch R., Breithaupt A., Mettenleiter T.C., Vahlenkamp T.W. Experimental infection and natural contact exposure of dogs with avian influenza virus (H5N1) Emerg. Infect. Dis. 2008;14:308–310.
35. Maas R., Tacken M., Ruuls L., Koch G., van Rooij E., Stockhofe-Zurwieden N. Avian influenza (H5N1) susceptibility and receptors in dogs. Emerg. Infect. Dis. 2007;13:1219–1221.
36. Reperant L.A., van Amerongen G., van de Bildt M.W., Rimmelzwaan G.F., Dobson A.P., Osterhaus A.D., Kuiken T. Highly pathogenic avian influenza virus (H5N1) infection in red foxes fed infected bird carcasses. Emerg. Infect. Dis. 2008;14:1835–1841.
37. Chen Y., Zhong G., Wang G., Deng G., Li Y., Shi J., Zhang Z., Guan Y., Jiang Y., Bu Z., et al. Dogs are highly susceptible to H5N1 avian influenza virus. Virology. 2010;15:15–19.
38. Moreno A., Bonfante F., Bortolami A., Cassaniti I., Caruana A., Cottini V., Cereda D., Farioli M., Fusaro A., Lavazza A., et al. Asymptomatic infection with clade 2.3.4.4b highly pathogenic avian influenza A(H5N1) in carnivore pets, Italy, April 2023. Euro Surveill. 2023;28:2300441.